Juvenile idiopathic arthritis, or JIA, is a chronic condition in children that causes joint inflammation, often affecting the feet and ankles. Foot involvement in JIA can lead to pain, swelling, stiffness, and difficulty walking. Over time, this inflammation may cause joint deformities or growth issues in the bones and soft tissues of the foot, affecting a child's mobility and quality of life. A podiatrist plays a key role in managing foot impairments in children with JIA. They can provide custom orthotics to support the foot, reduce pressure on affected joints, and improve walking comfort. Additionally, they may recommend exercises to maintain range of motion and suggest modifications to footwear to accommodate swelling or deformities. If you have a child with JIA, it is strongly suggested that you visit a podiatrist regularly to ensure foot issues are addressed early and long-term complications are prevented.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our doctors from New England Foot & Ankle . Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
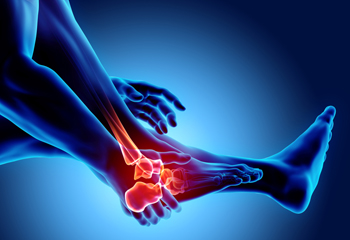
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Wakefield, MA, Nashua and Derry, NH . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.





